One of the biggest questions I had going into the refractive surgical practice was, “What in the heck is the difference between LASIK (Lay-sick), PRK, LASEK (Lay-sec), and SMILE” ?
First we should define each of these procedures and examine both the similarities and differences between them to understand why we have so many different procedures to achieve the same goal – improved Vision without the use of corrective lenses.
In this article series, we will outline each of these procedures, discuss the similarities and differences between them, as well as briefly introduce alternative or previously used procedures such as RK/AK, Clear Lens Exchange, Corneal Cross Linking, and Corneal Inlay procedures in their relation to refractive practices (which will be discussed more in depth in a later article series).
For a comprehensive history of these procedures please see the recommendations for readings at the bottom of each article along with and hyperlinks to cited source materials.
Each individual surgeon has their own personal preferences in terms of preoperative parameters and post operative outcomes that help to determine candidacy. The same goes for preoperative and post operative instructions, therefore it is important to check with your surgeon to find out what their personal preferences are – it should be noted this article should serve only as an educational reference and not a guide for that Allied health personnel.
Site Disclaimer
LASIK (Laser-Assisted In Situ Keratomileusis)
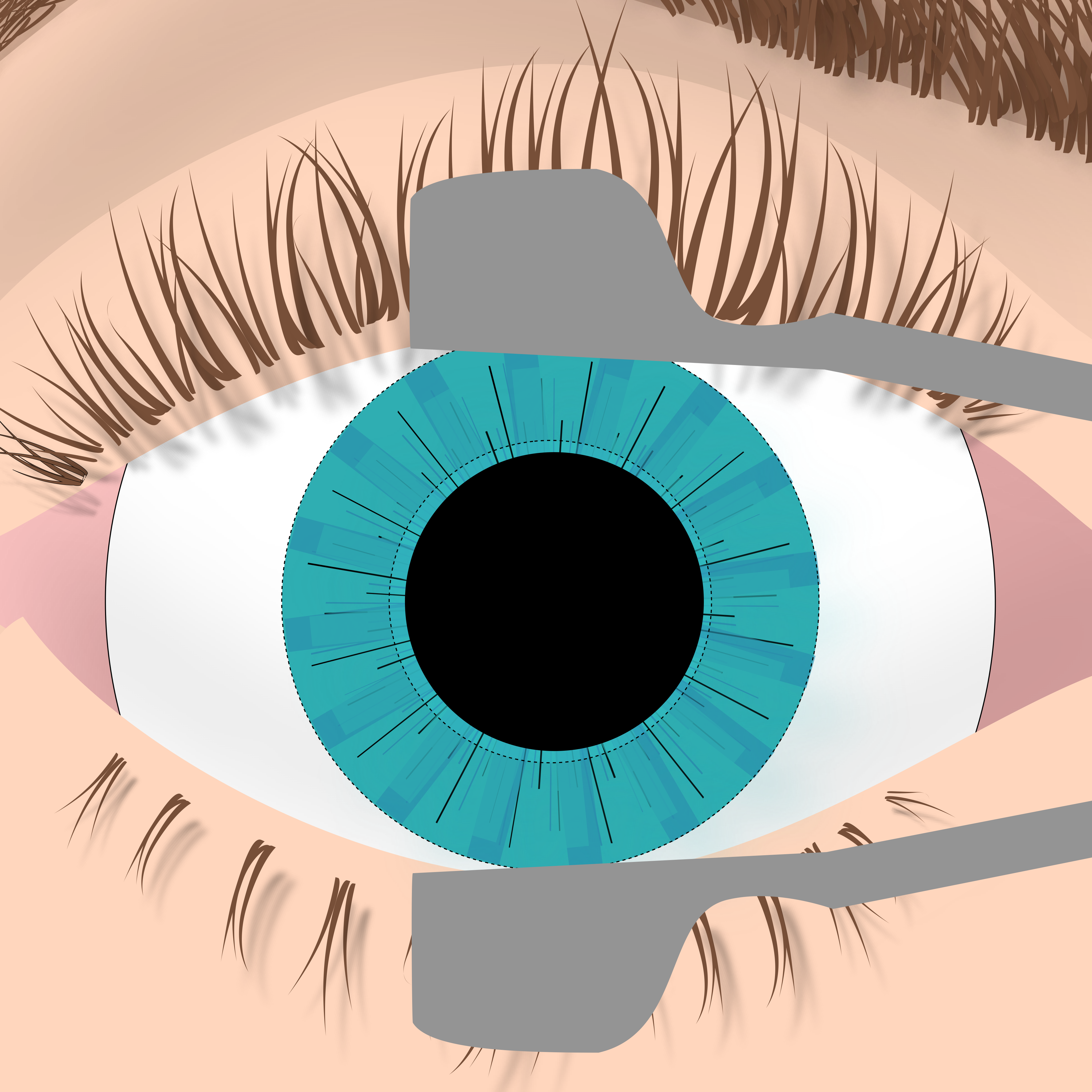
LASIK is the process of creating a hinged flap on the cornea, exposing the stroma to an excimer laser (Pulsating ultraviolet light laser) that will ablate (vaporize) tissue, effectively reshaping the cornea and moving the light’s focal point in the eye to the Macula. The flap is created by either a microkeratomb blade or a Femtosecond laser (all laser LASIK) and is moved out of the way for the excimer laser to reshape the corneal stroma. The flap is then folded back down over the newly shaped stroma and smoothed out, careful not to leave any folds, debris, air, or oil from the mebian Glands trapped beneath it. This is accomplished by using a cannula filled with BSS.
Learn more about LASIK !
PRK (Photorefractive Keratectomy)
The predecessor to modern LASIK, Photorefractive Keratectomy, abbreviated as PRK, is the process of removing just the epithelial layer of the cornea by one of two means. The epithelium can be removed either physically by a brush (looks like an electric toothbrush) that gently polishes the exterior of the cornea off, or chemically by an alcohol solution that is placed on the cornea for just a few seconds to loosen the epithelium, and then having it gently removed by the surgeon using either a tool or with a Spear. Once removed, the exposed stroma of the eye is ablated by the exclaimer laser. Often times a chemotherapy drug may be placed on the exposed post-ablated corneal tissue to reduce post operative haze while healing. Following the procedure a bandage contact lens is placed onto the eye for the 3-5 days while healing.
Learn more about PRK !
LASEK (Laser Assisted Sub-Epithelial Keratectomy)
LASEK is a procedure that resembles both PRK and LASIK. In LASEK, the epithelium of the cornea is loosened with alcohol, much like PRK, however instead of removing that epithelium completely, it is the folded over to expose the stroma much like a flap would be in LASIK. The corneal surface is then ablated with an excimer laser to move the convergent point of light in the eye onto the macula. The flap is then placed back onto the Corneal Surface and a bandage contact lens is placed over the cornea.
Learn more about LASEK !
SMILE (Small Incision Lenticule Extraction)
SMILE is a procedure that isolates tissue of the cornea, usually entering/exiting from the nasal and/or temporal sides, that would normally have been ablated in Lasik, and creating a lenticule (bag of tissue) that is removed. Once removed the epithelial layer on top will collapse down into the exposed lower layer of tissue, effectively sealing shut the opening.
Learn more about SMILE !
In some cases, none of the above refractive surgeries will be the best option for the patient due to prescription, age, quality of tear film, or other ocular/visual needs. A patient may be referred out for Corneal Cross linking prior to any refractive surgeries.
A patient with a very high prescription (outside of the range of some refractive surgeries) may seek out a Clear Lens Exchange (CLE) or Implantable Collamer Lens (ICL).
Allied Ophthalmology Health personnel may also encounter instances of Patients who may have had various Corneal inlays such as Raindrop Corneal Inlays. These corneal implant devices were used mainly to treat presbyopia patients, and are no longer approved for use in the United States.
Enter Table of Pros/Cons
Parameters can vary depending on the Surgeon and it is important to know what parameters your surgeon works in. However as a general rule patients with a difference in K value > 1.5D (superior – inferior values) Are considered at risk for corneal ectasia and May seek out other options.
Preoperative Considerations:
Because a patients overall systemic health and lifestyle habits can effect their healing and present potential postoperative challenges, an accurate history and complete examination is required to produce positive visual outcomes.
Potential tests that would be required to help your physician in determining the best type of surgery include:
– Auto Refraction (AR)
– Visual Acuity (VA’s) at Distance and Near both with (VA CC) and without Correction (VA SC)
– Lensometry (WRx)
– Confrontational Field Testing (CFT)
– Cover Testing (CT)
– Pupillary Examination (PERRLA +/- RAPD)
– Keratometry (K’s) / Topography (Topo)
– Pachyemetry (Pachy)
– Eye Dominancy (DOM)
– Tear Break Up Time (TBUT) or Schrimer Score
– Intraocular Pressure (IOP)
– Slit Lamp Exam (SL)
Some additional testing may also be required to rule out other ocular/visual abnormalities such as Axial Length (AXL) if the patient is Amblyopic, Endothelial Cell Microscopy (if the patient presents with thin Pachyemetry), or Visual Field Testing.
Often, Patients with Nystagmus, history of infectious disease (like Herpes for example), some autoimmune disorders, and those patients with other ocular/systemic diseases are not candidates for LASIK/LASEK/PRK or SMILE due to the risks of surgery potentially outweighing it’s benefits. Check with your doctor on what conditions are an automatic no-no for them.
Doctors will need to complete the full examination including both a “Dry” Manifest Refraction (MRx) and a “Wet” or Cycloplegic Refraction to determine the patients prescription prior to surgery. This is important because the Cycloplegic Or “Wet” refraction eliminates any accommodation of the lens and tells the surgeon how reliable the “Dry” Manifest Refraction is. The Surgeon Or OD should always be refining the Manifest prescription preoperatively to ensure accuracy as this is a major factor in planning for treatment.
Calculations that are important tools for the surgeon to take into consideration include the patients postoperative Residual Stroma Bed (RSB), and Percent of Tissue Altered/Ablated (PTA).
Ablation Depth & Optical Zone (often determined by the company that makes whichever exclaimer laser that is being used), Flap Thickness, and type of Microkeratome are left to Surgeon Preference which differ from Surgeon to Surgeon.
Post operative instructions may also vary from Surgeon to Surgeon however the following is a list of common instructions and why:
- Topical Broad spectrum antibiotics are often prescribed for the first week as a prophylactic against infection (commonly Moxifloxacin/Ofloxacin/Vigamox)
- Topical steroids are often prescribed to reduce inflammation- if your surgeon issues them for more than a few days they will likely have the patient taper off of them to prevent any dependency that may have developed with extended use. It should also be noted that with steroid use some patients may experience increases in their IOP and should be monitored for dangerous spikes at each post operative visit. Steroids also have a tendency to be in solution form (so the medication is solid and floating in a solution, like chocolate milk mix at the bottom of your glass before you stir it) and therefore patients need to be reminded to shake this medication before instilling it at home.
- Preservative Artificial Tears (PFAT’s) May be prescribed for relief of Dry Eye Symptoms (DES) that present following refractive procedures. It is important hat these are in individual vials and a multi dose bottle because the vials are single use (so there is less chance of infection transmission due to multiple use) and they do not contain any of the harsh preservatives that may cause pain or even hinder the healing process. Once the eye is healed however, the multi dose bottles can be used.
- Pain Management can be achieved many different ways and is entirely up to the Surgeon. Some may use oral medications for pain relief while others prefer to use topical Ketorolac (NSAID). The AAO Refractive Surgery Preferred Practices manual recommends using NSAID drops sparingly because, “drops may delay corneal epitheliazation”(it may slow down healing). Depending on the procedure and associated pain level the surgeon may also opt not to prescribe anything for pain
- For the first 24 hours following the Procedure, do not do anything strenuous with your eyes (I.e. watching tv/phone/computer/tablet/reading/driving etc.) It is not required to keep them closed for 24 hours however the patient should relax and keep them closed as much as possible.
- Limit physical activity for the first week of healing. This instruction may or may not including limiting actions such as waiting 1 week for sexual activity, lifting > 15-10 lbs, intensive cardio training, and even bending over from the waste. These restrictions are in place to reduce the chances of injury and to encourage the patient to rest while healing.
- No smoking! For at very least a week, smoke wreaks havoc all over the body but can really irritate the eyes. (And yes even marijuana/vape pens for my friends in states like California and Colorado)
- No rollercoasters, high speed wind force may damage a healing cornea
- It is very important to wear sun protection while healing (and in general). Glasses should be polarized, not just tinted to protect the eye from harmful UV rays and are only required to be worn outdoors. Patients who experience photophobia (light sensitivity) may wear them indoors to alleviate symptoms however for the majority of patients this is not required as most modern windows already filter harmful UV Rays (this is why Transition glasses don’t get dark inside).
- DO NOT RUB!!! For obvious reasons make sure the patient understands the importance of not rubbing their eye following corneal surgery (I.e. infection, improper healing, or acquiring new injuries). Discomfort can often be alleviated by the insertion of Preservative Free Artificial Tears (PFAT’s) can relive burning/itching sensations that may occur following surgery.
- Patients may choose to take additional Vitamin C and Omega3’s to help with healthy tear production (however the effectiveness of these supplements have been debated)
- The eye should not have pressure placed on it for at least a week following surgery and as such many surgeons may require patients to sleep in a clear plastic shield to prevent unconscious rubbing and keep the eye off of the pillows/blankets during sleep
- It is also important to remind patients about waiting at least 5 minuets in between instilling eye drops to prevent them from washing one another out
For patients outside the range of the above mentioned refractive surgeries not all is lost. Please check back in for the next article series covering Implantable Collamer Lens (ICL) & Clear Lens Exchange (CLE).
For patients not eligible due to different corneal disorders such as Kerataconus (KCN) or Pellucid Marginal Degeneration that are caught while screening for Refractive Procedures other options also exist. See our articles on Corneal Cross Linking (CXL), Corneal Inlays (Intacs), and Corneal Transplants (Keratoplasty).
